Welcome to the Podiatry Blog of Dr Richard Blake of San Francisco. I hope the pages can help you learn about caring for foot injuries, or help you with your own injury.
Total Pageviews
Translate
Followers
Saturday, March 12, 2022
Pronation Syndrome: The use of varus wedges for treatment and diagnosis
Friday, March 11, 2022
Beware of Subtle Xray Signs in the Foot
Thursday, March 10, 2022
Hallux Rigidus: Surgery, No Surgery, or In Between
Saturday, February 26, 2022
Sunday, January 30, 2022
Adding Stiffness to the front of a Shoe: Help for Many Problems in the Front of Our Feet
Monday, January 24, 2022
Chemotherapy Can Destroy Nails and Hair: Ice to the Rescue
Squeaking Orthotics: JSuede helps
Sunday, January 23, 2022
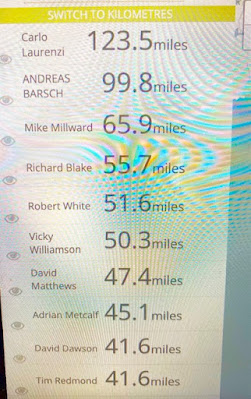
Virtual Walks are really fun!!!
Friday, January 21, 2022
Adding Stiffness to the Front of an Orthotic Device
Wednesday, January 19, 2022
Good Rx: A Good Way to Get Some Prescriptions at a fraction of the cost
Tuesday, January 18, 2022
Monday, January 17, 2022
Sunday Night Musings of a Personal Nature
Sunday, January 16, 2022
Lecturing: A Way of Giving Back
Thursday, January 13, 2022
Common Foot Pads used to Off Weight Sore Areas
Wednesday, January 12, 2022
MRIs: Their Usefulness in Patient Care of the Foot
Monday, January 10, 2022
LEMS: Shoes for Wide Feet
Sunday, January 9, 2022
Happy Birthday Me!!
Saturday, January 8, 2022
Customizing an OTC Insert: The list is endless and limited by our Imaginations!!
Thursday, January 6, 2022
Bunion Protection in Tight Shoes
Wednesday, January 5, 2022
Metatarsal Pads: Proper Placement
Sunday, January 2, 2022
Soccer Cleat and Foot Pain
Saturday, January 1, 2022
How Are We Built to Function? Loose and Unconnected, Perfect, or A-little of Both
Monday, December 27, 2021
Very Tight Tendons: Consider Heat Ice Prolonged Stretching
Sunday, December 26, 2021
Nerve Pain: Where Does It Come From?
Sunday, December 19, 2021
Podiatric Question #1
Practical Biomechanics Question #1: What position is the ankle in when it is the most relaxed, or the least stressed?
The ankle is the most relaxed at a 20-30 degrees plantarflexed pointed position and in Subtalar Neutral (neither pronated or supinated).
Plantar Fascia Healing of Partial Tear: 3 MRIs (6 months apart)
Big Toe Pain: Email Advice
I found your blog after dealing with chronic toe pain for the past 4 years. It started in 2017 when I was trying to stay healthy and did a bunch of yoga. I ended up doing a lot of hand stands and every time I would end I would plant my right great toe to the ground. Didn't start bothering me until I did some minimalist incline hiking.
Monday, December 13, 2021
Posterior Tendon Dysfunction: Email Advice
I’ve been reading your blog all day, thank you for proving this invaluable resource. I’ve been doing lots of research into posterior tibial tendon dysfunction and your site is a wealth of knowledge.
So I’ve been having some PTTD type problems. I ran an 73 mile ultra in July this year and really damaged the posterior tibial tendon. So much so I haven't been able to run properly since the injury. I’ve done some downhill walk running which was ok 5km ish. I have undergone reasonably intense physio protocol since September and I am now at the point where I am pretty much pain free day to day. I walk to work 45 minutes each way without pain, or with mild 1 or 2 pain on pain score.
Unfortunately my medial ankle started making a snapping sensation, which is worrying me. It feels like a ligament, possibly the PTT is snapping across the medial malleolus. Although it could be something to do with the deltoid ligament, this is where I notice the snapping sensation most, I am not sure of the cause. My PT gave me stretches and strengthening exercises, but the snapping only started occurring after I started rehabbing the injury. Now I am at the point where I am not sure if the tendon is loose and that’s causing the snapping or if it’s tight and that’s causing the snapping. There’s never an audible click as much, it’s more of a sensation you/I can feel. It can only be felt when the foot is dorsiflexed and inverted from the normal position upwards and inwards in that order. I sometimes notice the snapping when walking up hill. If the foot isn’t dorsiflexed and inverted then the snapping doesn’t happen.
My PT has helped, but isn’t a specialist in foot injuries, I can’t see a podiatrist until February and I am a mountaineer keen to get out as soon as possible. I was wondering if you had any advice regarding the snapping or ways to make the snapping stop? Everything I’ve found online in relation to snapping talks about the peroneal tendon, but that’s on the outside of the foot, and isn’t the source of my problem. I can’t find anything that specifically helps my inner foot snapping issue.
Best regards,
Monday, November 29, 2021
Treating Nerve Pain at the Foot: Algorithm
Sunday, November 28, 2021
Plantar Fasciitis: Treatment Algorithm
Tuesday, November 23, 2021
The 1 Day and 2 Day Pain Level Increase Rules of Rehabilitation
Saturday, November 6, 2021
Big Toe Area Pain: Years after Healing Sesamoid Injury
Hi Richard,I wanted to write to you because of pain in my big toe that has been bothering me for the past few weeks (about 5 weeks). Unfortunately, this pain is fickle and elusive, and very hard to describe.My history:- turf toe and sesamoid AVN in 2019-2020, which I recovered from thanks to your wonderful blog- I was walking perfectly fine for a ~6 months- played tennis one day and had pain the next day in my big toe, but a different one than I'd had before - it hasn't gone away unfortunatelyThe pain:The pain is sometimes very sharp when I put weight on my foot right after getting up, but then immediately subsides. At first it felt like "pins and needles", but now it hurts more "traditionally". I can't tell where exactly my toe is hurting, but it definitely hurts when I press in the webbing between the first and second toe. My joint clicks a bit (though when it does, it is painless), and to be honest I can't remember whether it did that before feeling the pain or not. Moving my big toe doesn't hurt, I have full range of motion, my sesamoids seem fine. It occasionally hurts when I compress my first phalanx with my hand, I think it's called the "proximal phalanx of the big toe". Overall the pain tends to be better in the morning, and worse after a whole day of walking.Please let me know if you have any leads, because I admit I'm quite perplexed by my current condition!May God preserve you and your family in this difficult time.With all my consideration
Dr Blake’s Comment: Thanks for your email and glad the sesamoid AVN finally healed and you were back to good activity. Some of the symptoms are definitely nerve, like the pins and needles and pain that comes on and disappears quickly. In your case, it could have just be the body trying to tell you that something is amiss that needs protection. Your original injury was to the big toe joint. Previous joint injuries tend to pop up from time to time. Like you are doing now, you have to take them seriously, but they represent that the joint is not perfect. Imperfect joints (for me they are the left ankle, right knee, low back, and right shoulder) from old injuries are generally alittle stiffer (so they can get jerked easier) and the body’s reaction is quicker (from nerve memory).
So, what does this all mean? Typically, we are not dealing with anything serious if the range of motion is normal and there is no swelling, black and blue, or redness. Also, it is a great sign that there are times of the day that it does not hurt at all. These aggravations of old injury areas need to be treated seriously since this joint is a weak spot for you. The 3 areas to address are mechanics, probably spica taping or bunion toe separators to start, inflammation (so icing and contrast bathing once or twice daily), and nerve hyper-sensitivity (neural flossing with non painful joint motions, and non painful massage for 2 minutes twice daily. This should be done for 2 weeks, and then based on the response, either lessen your treatments or increase them in some way.
I hope this makes sense. Rich