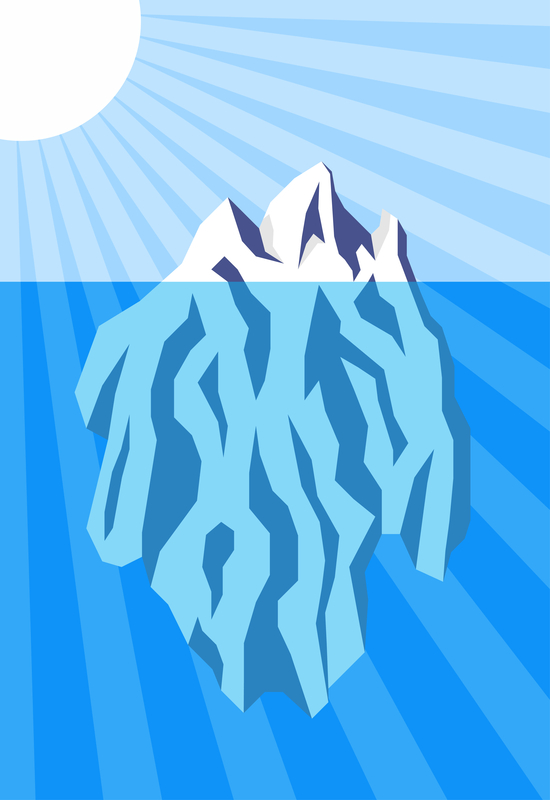
Each week I have patients that present with their first foot or ankle injury and I wonder whether I am looking at the Tip of the Iceberg of this and other future injuries. No matter how minor the injury appears, I wonder if it will be followed by another and another and another. What can I do as a healthcare provider to eliminate or at least minimize the onslaught of future injuries? How serious should I take these initial injuries which will heal relatively quickly? Should I always follow the KISS Principle and Keep It Simple Stupid when I think some of these injuries are definitely the Tip of the Iceberg? More pain is on the way. What goes into the thought process of deciding who should get more treatment when relatively simple injuries present into my office? The treatment of any overuse injury (without an acute single episode) should always be directed at the one or two common causes, or the several possible causes for this individual patient. Take Achilles Tendonitis for example. The common causes of Achilles Tendonitis are:
1. Straight overuse situation in which the Achilles Tendon is put in major stress (i.e. stair running for the first time, or working out too many days in a row, etc.)
2. Very tight Achilles Tendons.
3. Worn out shoe gear with lack of stability or cushion at impact.
4. Unstable shoes, or excessive wearing of shoe gear with inadequate support (i.e. too much time in the flip flops, etc.)
5. Short leg with compensation of early heel lift.
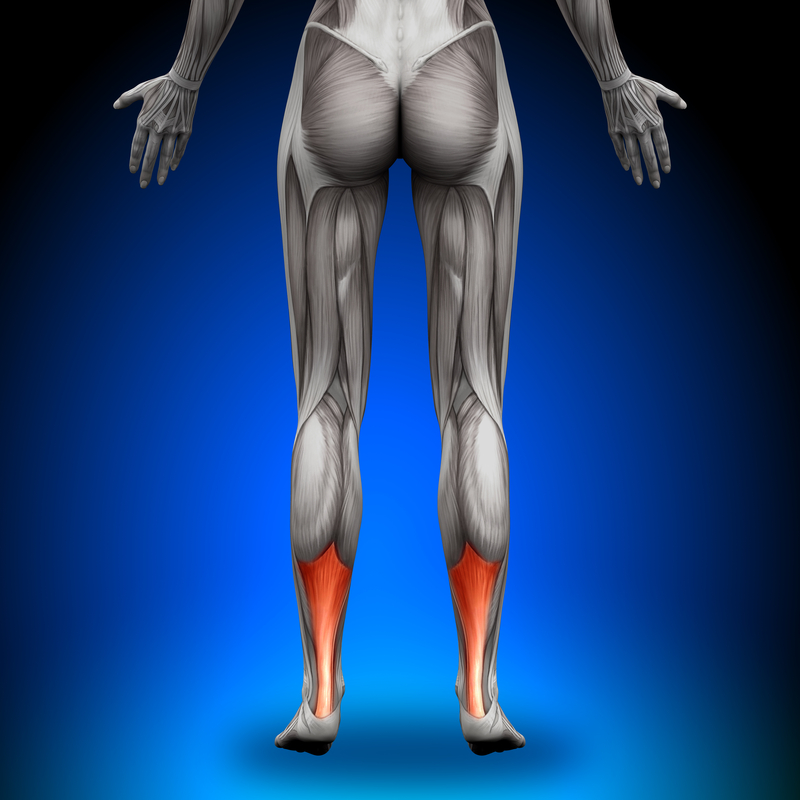
6. Excessive pronation of the foot/ankle with excessive torque on the Achilles (as seen in the left foot of the photo below).
7. Excessive supination of the foot/ankle with lateral instability and over firing of the Achilles Tendon to stabilize the ankle joint complex.
8. Very loose Achilles Tendons from over stretching or patients with loose ligaments in general. This produces a weakness in the tendon (see future post on the force/length curve).
9. Weak Achilles Tendons from many reasons (just returning to regular exercise program, following prolonged casting, aging process, genetics, dietary, etc.)
10. Achilles Tendonitis secondary to another problem (heel spurs, ankle injuries, sciatica, tibial stress fractures, etc.)
After performing an initial history and physical examination, and making the diagnosis if possible, the clinician will try to assess the reasons this individual patient developed their injury. It is the experience of the clinician that separates them from other health care providers in getting to the cause(s) of some injuries. Some “reversal of cause” treatment must be initiated in all cases. But for some patients, looking below the surface level of water, below the Tip of the Iceberg, is really what is crucial. What factors could lead, if not addressed, to either prolonged injury/treatment, or frequent recurrences of the symptoms. This is so crucial, but in a busy medical practice, often times not proactively explored. The patient and clinician only stumbles into the discoveries.
When a ship’s captain looks at the iceberg approaching, the captain scrutinizes the situation, assesses the severity, and then makes an appropriate plan. Health care providers, and proactive patients, can be slower than the sea captain at finally making these decisions, but must look at possible severity of the injury, and severity of the cause of injury, to come up with an appropriate plan. Since we can grade the severity of anything 3 typical ways—mild, moderate, and complex—let us look at these 2 factors in injury treatment from this angle. Perhaps then you can understand when under the Tip of the Iceberg danger may be lurking in the forms of prolonged treatment, possible incomplete healing, and frequent recurrences of the symptoms. After the initial assessment (history and physical), and perhaps after several follow up visits, the clinician will place the patient in one of 9 categories. These are:
1. Mild Injury/Mild Severity of Cause
2. Mild Injury/Moderate Severity of Cause
3. Mild Injury/Complex Severity of Cause
4. Moderate Injury/Mild Severity of Cause
5. Moderate Injury/Moderate Severity of Cause
6. Moderate Injury/Complex Severity of Cause
7. Severe Injury/Mild Severity of Cause
8. Severe Injury/Moderate Severity of Cause
9. Severe Injury/Complex Severity of Cause
With the Severe Injuries, the treatment is usually prolonged enough that the patient and doctor/therapist gradually work at recognizing and correcting all possible causes of the injury along the way. It is the Mild and Moderate Injuries, that the KISS principle and Tip of the Iceberg principles must be reconciled. It is when the injury is classified as mild or moderate that the health care provider must decide when to look under the Tip of the Iceberg and explore the depths of moderate to complex causes. It is in the 4 categories below that I find most problems in dealing with these injuries. These are:
1. Mild Injury/Moderate Severity of Cause
2. Mild Injury/Complex Severity of Cause
3. Moderate Injury/Moderate Severity of Cause
4. Moderate Injury/Complex Severity of Cause
In these cases, I see the most patients for 2nd opinions. Why is the injury not healing? Why does the injury keep coming back? The mild and moderate nature of the initial injury makes the healthcare system relax and not look too deep into cause of injury.
I will end this discussion with one example of this dilemma. Since I already used Achilles Tendonitis above, I will finish using an example of Achilles Tendonitis. The patient had pain in the Achilles for 3 months prior to seeing the initial doctor. The patient was a runner who pronated too much, rarely stretched the Achilles, when stretching only did Negative Stretching off a curb (which I do not encourage), was a vegetarian (not to pick on you guys too much!) but ate well, ran a lot of hills after moving from Dallas to San Francisco, and was told he had one leg shorter but never did anything about it. The initial treatment addressing the possible causes of the injury were Orthotic devices for the pronation, new motion control running shoes, power lacing, Achilles stretching 3 to 5 times a day, and running on flat ground, not hills until the symptoms got better. The doctor had categorized the patient mild injury/moderate cause of injury and had addressed the causes on the surface well. Was he/she just looking at the Tip of the Iceberg? What was below the surface that needed to be addressed? The patient after six months of treatment still was not much better in function. Running was still very limited. The initial treating doctor told him to stretch more and give it more time at their last visit (of 6 visits overall). This patient then sought a 2nd opinion.
On review of the injury itself, the right diagnosis had been made. The plan of treatment initiated was good, but never improved upon when the patient was struggling. Each of the treatments initiated were subpar in retrospect. The pronation was only partially corrected with the new Orthotic devices (but they were easy to modify to greatly improve their function), the running shoe store had convinced him to not get a motion control shoe since he had Orthotic devices (and the doctor never evaluated his running after the first visit), the power lacing has been done incorrectly (and was also modified), diet counseling came up with non optimal protein intake (something that will help the patient forever), measurement of his flexibility showed him off the charts in over flexibility (too flexible means too weak and this was improved with 6 weeks of no stretching at all—he thought I was crazy when I proposed that one), and exact measurement of his legs showed over ½” short leg on the injured side (treatment with heel lifts helped him immensely). Within several weeks, he was feeling much better, and by 8 weeks was back running regularly with a better diet, heel lift for the short leg, sensible stretching routine before and after exercise, no negative achilles stretching, stable Orthotic devices, stable shoes, proper power lacing, and a gradual re-strengthening home program under a physical therapist with 6 one/month visits to up the ante. Yes, under the Tip of the Iceberg for this athlete was a considerable short leg, a considerable dietary problem, slightly harder to treat pronation, and an Achilles that could become over flexible too easily. His mild injury did not initially respond since the cause of injury was misread as moderate, when it really was complex.
The Golden Rule of Foot: When treating athletic injuries, if the symptoms and function plateau, look under the Tip of the Iceberg to a deeper level of possible answers.
